Condyloma acuminate is a skin-colored fleshy wart caused by the Human Papillomavirus (HPV). The disease is typically asymptomatic, but in rare cases, it can be sexually transmitted or acquired through autoinoculation of the maternal genital tract. In a pregnant woman, the lesions are most likely to develop on the lips, cheeks, and hard palate.
Various treatments are available for condyloma acuminatata, which is a complication of the human papillomavirus. Because condyloma can recur even after topical therapies, patients are often referred to a plastic surgeon for surgical excision. Although this is a rare cause of the disease, it should always be investigated thoroughly.
As with other sexually transmitted diseases, treatment options for condyloma acuminatum are individualized, and the best treatment will depend on each patient’s unique case and response to previous treatments. Some treatments are topical and non-surgical, while others require surgical excision. The type of treatment should depend on the location and morphology of the lesions, and the preference of the patient.
Treatment for condyloma acuminatata is tailored to each individual’s situation. If the lesions are small or asymptomatic, treatment is not urgent. They often resolve spontaneously over months or even years. However, in patients who are concerned about the cosmetic appearance of the lesions, treatment should be pursued. There are several treatments available, including cryotherapy, topical therapy, and surgical excision. Surgical excision is the most effective treatment for condyloma acuminala, but it is rarely successful.
Treatment for condyloma acuminatata involves a number of different procedures. Some patients may be able to cure themselves with topical treatments, while others may require surgical excision. For patients with advanced lesions, surgery is usually the only option. But the recurrence rate of the condition is higher after a single treatment. For such patients, it is best to seek treatment for condyloma acuminala.
Symptomatic condyloma can be difficult to detect without a biopsy. In patients with the condition, medical treatment is necessary to prevent the recurrence of the lesion. In addition, patients should be warned about the possible risks of sex with people with condyloma. During the course of treatment, a physician should present all treatment options available. If the lesions are extensive, the patient may need more than one course of therapy.
The best treatment for condyloma acuminatata is an indeterminate disease that may be caused by the human papillomavirus (HPV). This disease affects the genital and perianal mucosae, as well as the urethral mucosa. The most common form of treatment is excision, although some people may have a recurrence after a single treatment.
Treatment for condyloma acuminatata varies in severity and is based on the patient’s preference. In children and young adults, the treatment for condyloma requires a thorough evaluation to identify the disease. A doctor will also consider the age of the patient. While the disease is rare in women, it can develop in men. Moreover, it is more common in males than in females.
Acute genital warts is a minor growth that usually disappears on its own. Affected individuals may experience bleeding or itching. Despite the relatively low recurrence rate, the disease is incurable. Although most patients will not have symptoms of warts, it can be treated. Several treatment options are available to the patient. You can find more information about the possible treatment options for genital warts on the website observatoriojovenes.com.ar.
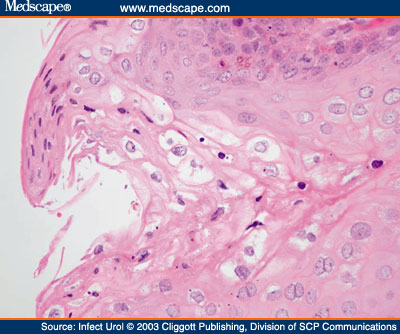
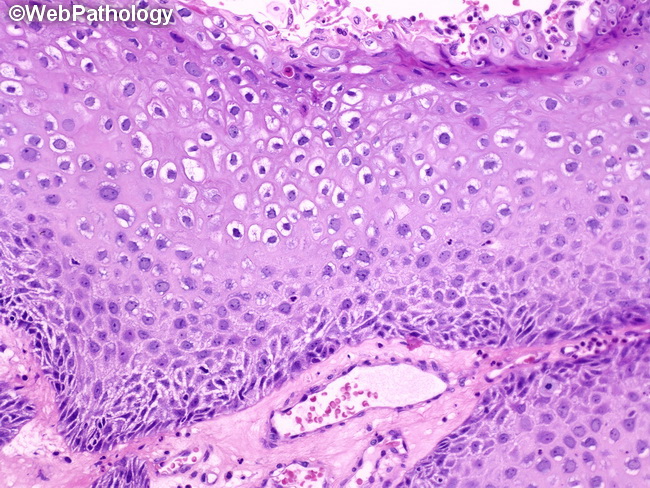
The biopsy showed that the lesions measured 12×5 cm and were acanthotic. The foci were localized in the perianal region, the right and left labia minora and the clitoris. The cervix and upper vagina were normal. The patient had a cervical smear, which was negative for papilloma. This was confirmed by a biopsy.
The patient underwent a simple vulvectomy under spinal anesthesia. The foci on the large and small labia are excised. Eruptions in the perianal areas were cauterized. A 2-0 Vicryl suture was used to close the wound. Two days later, the woman was able to return home on her own, but it was difficult to return her after the operation.

Leave a Reply